Cannabis, also known as marijuana (from the Mexican Spanish marihuana), and by numerous other names,a is a preparation of the Cannabis plant intended for use as a psychoactive drug and as medicine. Pharmacologically, the principal psychoactive constituent of cannabis is tetrahydrocannabinol (THC); it is one of 483 known compounds in the plant,including at least 84 other cannabinoids, such as cannabidiol (CBD), cannabinol (CBN), tetrahydrocannabivarin (THCV). and cannabigerol (CBG).
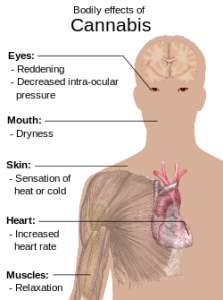
Cannabis is often consumed for its psychoactive and physiological effects which can include heightened mood or euphoria, relaxation, and increase in appetite. Unwanted side-effects can sometimes include a decrease in short-term memory, dry mouth, impaired motor skills, reddening of the eyes, and feelings of paranoia or anxiety.
Contemporary uses of cannabis are as a recreational or medicinal drug, and as part of religious or spiritual rites; the earliest recorded uses date from the 3rd millennium BC. Since the early 20th century cannabis has been subject to legal restrictions with the possession, use, and sale of cannabis preparations containing psychoactive cannabinoids currently illegal in most countries of the world; the United Nations has said that cannabis is the most-used illicit drug in the world.In 2004, the United Nations estimated that global consumption of cannabis indicated that approximately 4% of the adult world population (162 million people) used cannabis annually, and that approximately 0.6% (22.5 million) of people used cannabis daily.
Effects
Cannabis has psychoactive and physiological effects when consumed. The immediate desired effects from consuming cannabis include relaxation and mild euphoria (the “high” or “stoned” feeling), while some immediate undesired side-effects include a decrease in short-term memory, dry mouth, impaired motor skills and reddening of the eyes.Aside from a subjective change in perception and, most notably, mood, the most common short-term physical and neurological effects include increased heart rate, increased appetite and consumption of food lowered blood pressure, impairment of short-term and working memory, psychomotor coordination, and concentration. Long-term effects are less clear. In humans aside from respiratory damage when smoked, relatively few adverse clinical health effects have been documented from chronic cannabis use.
Psychoactive Classification
A 2010 study published in the Journal of Health and Social Behavior found that the main factors in users moving on to other drugs were age, wealth, unemployment status, and psychological stress. The study concluded that there is no validity to the “gateway theory” and that drug use is more closely tied to a person’s life situation, although cannabis users are more likely to use other drugs.[67]While many psychoactive drugs clearly fall into the category of either stimulant, depressant, or hallucinogen, cannabis exhibits a mix of all properties, perhaps leaning the most towards hallucinogenic or psychedelic properties, though with other effects quite pronounced as well. THC is typically considered the primary active component of the cannabis plant; various scientific studies have suggested that certain other cannabinoids like CBD may also play a significant role in its psychoactive effects.
Medical Use
Cannabis used medically has several well-documented beneficial effects.Among these are: the amelioration of nausea and vomiting, stimulation of hunger in chemotherapy and AIDS patients, lowered intraocular eye pressure, as well as general analgesic effects (pain reliever). Less confirmed individual studies also have been conducted indicating cannabis to be beneficial to a gamut of conditions running from multiple sclerosis to depression. Synthesized cannabinoids are also sold as prescription drugs, including Marinol (dronabinol in the United States and Germany) and Cesamet (nabilone in Canada, Mexico, the United States and the United Kingdom).
Currently, the U.S. Food and Drug Administration (FDA) has not approved smoked cannabis for any condition or disease in the United States, largely because the FDA claims good quality scientific evidence for its use from U.S. studies is lacking.Others, for example American Society of Addiction Medicine, argue that there is no “Medical marijuana” because the plant parts in question fail to meet the standard requirements for approved medicines.
Eighteen states and the District of Columbia have legalized cannabis for medical use in state laws. The United States Supreme Court has ruled in United States v. Oakland Cannabis Buyers’ Coop and Gonzales v. Raich that it is the federal government that has the right to regulate and criminalize cannabis, even for medical purposes and even if the state legalize it. Canada, Spain, The Netherlands, France, Italy, Czech Republic and Austria have legalized some form of cannabis or extract containing a low dose of THC for medicinal use. Recently, Uruguay has taken steps towards legalising and regulating the production and sale of the drug.
Other Effects
Though the long-term effects of cannabis have been studied, there remains much to be concluded. Many studies have investigated whether long-term use of cannabis can cause or contribute to the development of illnesses such as heart disease, bipolar disorder, depression, mood swings or schizophrenia. Its effects on intelligence, memory, respiratory functions and the possible relationship of cannabis use to mental disorders such as schizophrenia, psychosis,depersonalization disorder and depression are still under discussion.
Both advocates and opponents of cannabis are able to call upon numerous scientific studies supporting their respective positions.For instance, while cannabis has been implicated in the development of various mental disorders in some studies, these studies differ widely as to whether cannabis use is the cause of the mental problems displayed in heavy users, whether the mental problems are exacerbated by cannabis use, or whether both the cannabis use and the mental problems are the effects of some other cause.
It has been pointed out that as cannabis use has risen, rates of schizophrenia have not risen in tandem. Lester Grinspoon argues that the cannabis-causes-psychosis argument is disproved by the lack of “even a blip in the incidence of schizophrenia in the US after millions of people started smoking marijuana in the 1960s”. Worldwide prevalence of schizophrenia is about 1% in adults; the amount of cannabis use in any given country seems to have no effect on that rate.
A medical study published in 2009 taken by the Medical Research Council in London, concluded recreational cannabis users do not release significant amounts of dopamine from an oral THC dose equivalent to a standard cannabis cigarette, and that therefore cannabis use could leave users vulnerable to psychosis.
Addictiveness
Dr. Jack E. Henningfield of NIDA ranked the relative addictiveness of 6 substances (cannabis, caffeine, cocaine, alcohol, heroin and nicotine). Cannabis ranked least addictive, with caffeine the second least addictive and nicotine the most addictive.
Adolescent Brain Development
A 35-year cohort study published August 2012 in Proceedings of the National Academy of Sciences and funded partly by NIDA and other NIH institutes reported an association between long-term cannabis use and neuropsychological decline, even after controlling for education. It was found that the persistent, dependent use of marijuana before age 18 was associated with lasting harm to a person’s intelligence, attention and memory, and were suggestive of neurological harm from cannabis. Quitting cannabis did not appear to reverse the loss. However, individuals who started cannabis use after the age of 18 did not show similar declines.
Results of the study came into question when in a new analysis, published January 2013 in Proceedings of the National Academy of Sciences, researchers from Oslo’s Ragnar Frisch Center for Economic Research noted other differences among the study group including education, occupation and other socioeconomic factors that showed the same effect on IQ as cannabis use. From the abstract: “existing research suggests an alternative confounding model based on time-varying effects of socioeconomic status on IQ. A simulation of the confounding model reproduces the reported associations from the [August 2012 study], suggesting that the causal effects estimated in Meier et al. are likely to be overestimates, and that the true effect could be zero”. The researchers pointed to three other studies which showed cannabis did not cause a decline in IQ. The studies showed that heavy smokers had clear reductions in IQ, but they were not permanent.
A July 2012 article in Brain reported neural-connectivity impairment in some brain regions following prolonged heavy cannabis use initiated in adolescence or young adulthood.
A 2012 study conducted by researchers at UC San Diego failed to show deleterious effects on the adolescent brain from cannabis use. Researchers looked at brain scans taken before-and-after of subjects aged 16–20 years who consumed alcohol and compared them to subjects of the same age who used cannabis instead. The 92 person study was conducted over an eighteen-month period. While teen alcohol use resulted in observable reduced white matter brain tissue health, cannabis use was not linked to any structural damage. The study did not measure the subjects’ cognitive performance.The study has been publicized in Alcoholism: Clinical and Experimental Research on January 2013.
Gateway Drug Theory
Since the 1950s, United States drug policies have been guided by the assumption that trying cannabis increases the probability that users will eventually use “harder” drugs. This hypothesis has been one of the central pillars of anti-cannabis drug policy in the United States, though the validity and implications of this hypothesis are hotly debated. Studies have shown that tobacco smoking is a better predictor of concurrent illicit hard drug use than smoking cannabis.
No widely accepted study has ever demonstrated a cause-and-effect relationship between the use of cannabis and the later use of harder drugs like heroin and cocaine. However, the prevalence of tobacco cigarette advertising and the practice of mixing tobacco and cannabis together in a single large joint, common in Europe, are believed to be cofactors in promoting nicotine dependency among young people trying cannabis.
A 2005 comprehensive review of the literature on the cannabis gateway hypothesis found that pre-existing traits may predispose users to addiction in general, the availability of multiple drugs in a given setting confounds predictive patterns in their usage, and drug sub-cultures are more influential than cannabis itself. The study called for further research on “social context, individual characteristics, and drug effects” to discover the actual relationships between cannabis and the use of other drugs.
Some studies state that while there is no proof for this gateway hypothesis, young cannabis users should still be considered as a risk group for intervention programs. Other findings indicate that hard drug users are likely to be “poly-drug” users, and that interventions must address the use of multiple drugs instead of a single hard drug.
Another gateway hypothesis is that a gateway effect may be detected as a result of the “common factors” involved with using any illegal drug. Because of its illegal status, cannabis users are more likely to be in situations which allow them to become acquainted with people who use and sell other illegal drugs. By this argument, some studies have shown that alcohol and tobacco may be regarded as gateway drugs. However, a more parsimonious explanation could be that cannabis is simply more readily available (and at an earlier age) than illegal hard drugs, and alcohol/tobacco are in turn easier to obtain earlier than cannabis (though the reverse may be true in some areas), thus leading to the “gateway sequence” in those people who are most likely to experiment with any drug offered.
A 2008 study at Karolinska Institute suggested that young rats treated with THC received an increased motivation for drug use, heroin in the study, under conditions of stress.
A 2010 study published in the Journal of Health and Social Behavior found that the main factors in users moving on to other drugs were age, wealth, unemployment status, and psychological stress. The study concluded that there is no validity to the “gateway theory” and that drug use is more closely tied to a person’s life situation, although cannabis users are more likely to use other drugs.